RNA: Your New Favorite Messenger
The Future of Pharmaceuticals
By Valkyrie Holmes

On March 5th, 2015, the Bill and Melinda Gates Foundation pledged $52 million dollars to a German biopharmaceutical company named CureVac.
Since it’s creation in 2000, it has become the leading company in research concerning DNA and RNA and has since had more than $24 million dollars invested into it since 2015.
Throughout the COVID-19 outbreak, multiple bioengineering companies have been trying to come up with a vaccine for the virus- and fast.
If we can teach the body to create its own natural defenses, we can revolutionize the way we treat and prevent diseases. Technologies like mRNA give us confidence to place big bets for the future. — Bill Gates
Many have promising results: NovaVax is testing a non-infectious version of the virus to inject into the human body just like the flu vaccine. Sinopharm in China is testing an inactivated SARS virus for protection against the Coronavirus. Gamaleya in Russia is using a weakened strain of adenovirus (the virus that causes the common cold).
It seems that everyone is head to head, racing to find a cure.
So what’s so special about one German company?
CureVac, along with its partner companies, BioNTech and Moderna Therapeutics, has found a way to enhance the body’s natural systems to fight back against diseases, and they’re doing it with the help of our favorite messenger: RNA.
It’s called the RNA Impfungen, or the RNA vaccine in English, and the possibilities are seemingly endless.
Why RNA?
You may be wondering, why can’t we just use DNA for vaccines? What about RNA makes this so revolutionary?
First off, normal DNA vaccines and RNA vaccines are similar but RNA is much cheaper and faster to produce as well as being safer to the patient. DNA vaccines have to penetrate the cytoplasm and the nucleus, whereas RNA vaccines only have to penetrate the cytoplasm. This way, there’s no way injecting RNA can disrupt the natural DNA sequence of the cells.

How Does It Work?
Now, you may not remember how regular vaccines work so let me refresh your memory with the most common annual vaccine- influenza.
When the vaccine is injected, it introduces something called an antigen into the body. Antigens are toxins that elicit an immune response, not to be confused with pathogens, which are bacteria, viruses, or microorganisms that cause disease.
When we train the immune system, we use dormant pathogens as antigens. By presenting the body with these antigens, it stimulates the immune system, specifically antibodies, who have the ability to remember the inactivated disease and store data on how to deal with it at a later date.
It’s basically like teaching a system how to solve a problem and giving it that same problem over and over again until it can effectively pass the test.
Think of antigens as the villains and antibodies as the heroes, coming to save the day whenever the bad guy strikes again!
This has been effectively used for decades to teach cells how to fight infections and has eradicated diseases like smallpox and polio.

Now here’s where RNA comes in.
DNA is arranged in a series of base pairs that code for certain proteins to be made inside the cell. mRNA carries that information to a ribosome inside the cell, which arranges an amino acid and the genetic code into a certain protein.
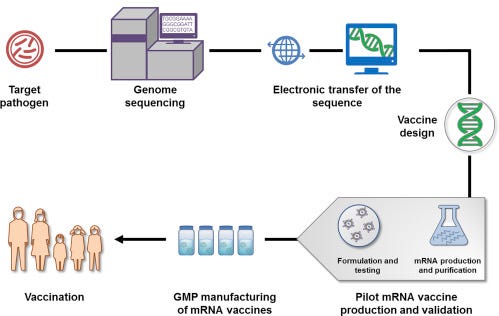
An RNA vaccine introduces a specifically coded mRNA sequence (for a specific antigen) into the cell. Because the genetic code is embedded into the RNA, it comes in contact with a ribosome and turns that sequence into the required antigen.
Contrary to a regular vaccine, no antigen is actually released into the body. Instead, the RNA gets the information needed to create the antigen on its own. It then synthesizes that information to make the dormant pathogen, triggering the antibodies of the immune system like a normal vaccine would.
So now, the RNA is the go-between agent for our main protagonist; he gets the right location of the villain to the superhero and with that new information, the man of the hour can fight to save the city!
Types of RNA Vaccines
The vaccine can be delivered via needle injection or via nasal spray and there are multiple types in the works.
- Non-Replicating RNA: the simplest method; a strain inserted into the body to make the antigen.
- In Vivo Self Replicating RNA: mRNA strands are packed together with additional RNA sequences to make sure that it can be copied once inside the cell. This second method creates a more heightened immune response.
- In Vitro Dendritic Cell Non-Replicating RNA: This one sounds daunting but is actually quite simple. The process consists of extracting a patient’s blood and injecting the cells with the mRNA first and then reintroducing it into the body to spike an immune response.
In the past, in vitro vaccination has been deemed unstable and inefficient. But as time goes on and more research is done on safely transporting the vaccine into the body, we get closer and closer to using this system in all areas of medicine.
Pros and Cons
In a 2019 study done by the Multidisciplinary Digital Publishing Institute (MDPI), they did an in-depth comparison of DNA vaccines and RNA vaccines and found that on top of the RNA vaccine not having to go inside the nucleus, the number of protein antigen molecules created was amplified. The antigen spread farther than it did in DNA vaccine studies.
In RNA vaccines, only the expression of the antigen must be made. When the whole antigen protein doesn’t have to be produced, it cuts the cost of the vaccine dramatically. The dosage is also significantly lower, almost 1000 times lower on average, in fact.
While all these effects are certainly promising, there are things we need to be aware of in terms of mRNA.
Sometimes, the injected strand of mRNA may cause an unwanted immune response and RNA must be incorporated into a larger molecule to help stabilize it in order to move into the body safely. It’s also hard to keep RNA vaccines refrigerated in developing countries where these kinds of technology may not be available.
The FUTURE Is Here
In sudden pandemics, like COVID-19, the time that it would take to make a vaccine targeting the disease would be cut down significantly, with the leading company CureVac claiming they could have vaccines out in two months to cut production costs (though it’s still being heavily researched before it can be safely released).
Its specifically being looked into for “cancer vaccines”, where specific markers are coded into the RNA to make the immune system attack the tumors themselves. The variability of tumors makes this hard to study, however, and it’s still being developed. There is also work in teaching cells to fight infectious diseases, like HIV, the flu, and rabies, although those are all still in the research stages.

mRNA vaccines are the future of pharmaceuticals and in order to make it accessible to everyone, a lot more research must be done to safely pass it along. But every month, we get closer and closer to unlocking these possibilities.